CPR in Traumatic Arrest
*Disclaimer: I am not a trauma surgeon. I am not in charge of these resuscitations. My home institution did not do CPR during the vast majority of trauma codes.*
Question: What is the role of CPR in traumatic cardiac arrest?
The key in traumatic arrest is prioritizing the immediate treatment of reversible causes (hypoxia, hypovolemia, tension PTX, tamponade) to allow re-establishment of effective coronary blood flow. This should take priority over chest compressions.
Chest compressions can be initiated before reversible causes are addressed if we have enough resources to deliver high quality CPR and they do not hinder immediate management of reversible causes.
If the traumatic arrest is from a non-hypovolemic, non-obstructive cause (isolated TBI, asphyxiation, drowning), then yes, proceed with CPR.
Rationale:
To achieve ROSC and maintain cardiac activity, we need to maintain coronary artery perfusion. In your non-hypovolemic, non-obstructive codes (or medical codes), CPR increases aortic diastolic blood pressure and allows for the generation of a pressure gradient to perfuse the coronaries.
External compressions are not effective in traumatic cardiac arrest that results from hypovolemia or obstruction. These etiologies prevent sufficient coronary artery perfusion even with compressions.
Basically (these are my words): what blood are we circulating if it’s not in the vasculature, but rather in a body cavity, or on the floor???
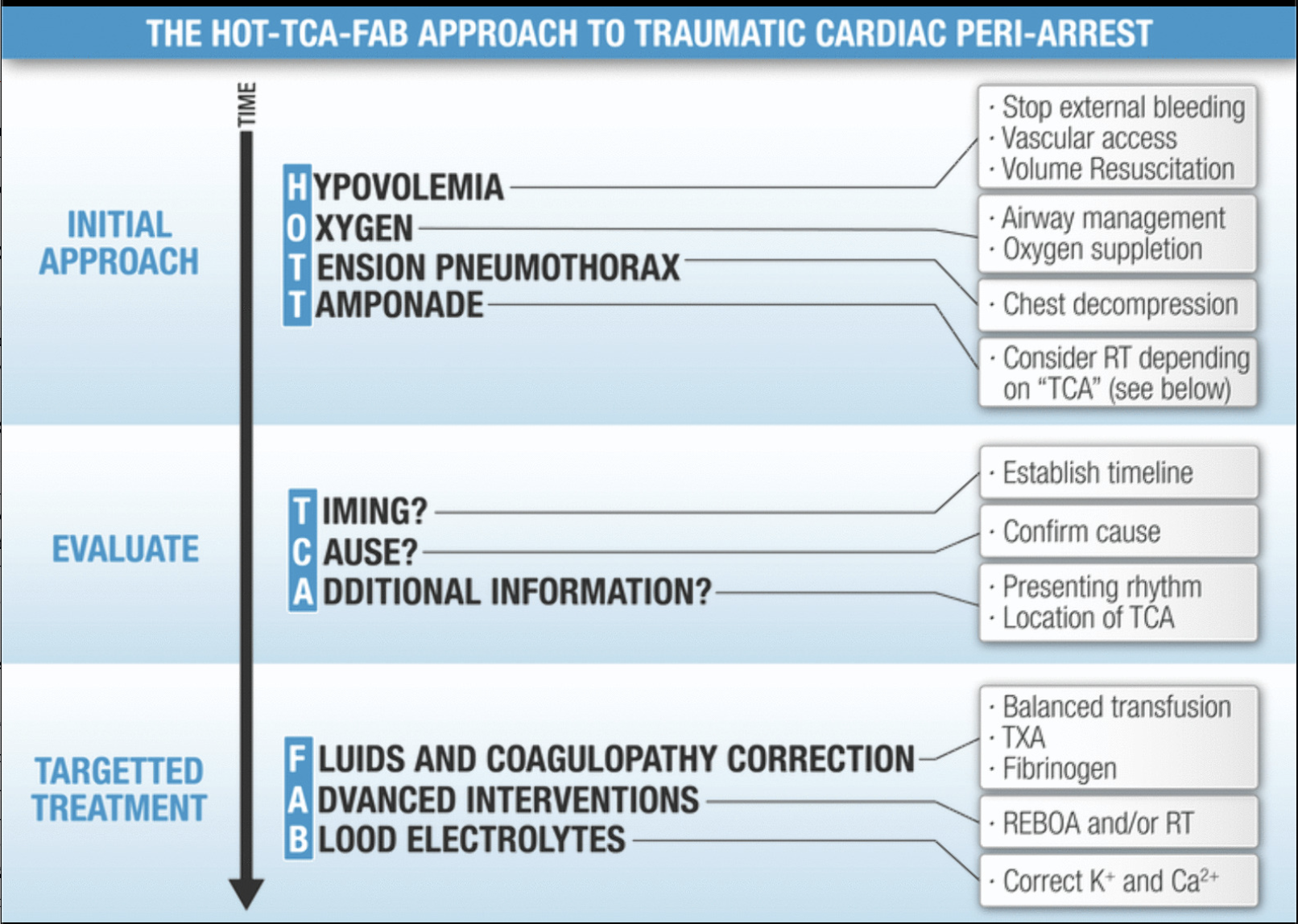
Initial Approach to the Traumatic Cardiac Arrest
Carenzo et al, 2025
1. Stop bleeding, get access, volume resuscitate (Hypovolemia)
Preferably blood, in 1:1:1 (maybe whole blood)
Large bore IV access
2. Manage the airway and give O2 (Hypoxia)
Consider BVM/LMA if intubation manpower/resource intensive
3. Decompress the chest (Tension PTX)
Finger preferred over needle due to success rates
4. Consider Resuscitative Thoracotomy (Tamponade).
If the compressor is preventing the procedure doc from doing these procedures (decompressing the chest)—the trauma leader should tell the compressor to stop compressions. It also is unsafe for the team (scalpels around compressing, bouncing hands) and thus an unnecessary risk.
For a blunt traumatic arrest (based on this review article), best practice would be:
EMS comes in. Then simultaneously–
IV access and fluids/blood started by nursing
Trauma Resident is on airway and gets a definitive airway.
Bilateral finger thoracostomies by the ED and surgery
Arrest in the ED or arrest within 5 mins, can consider thoracotomy
These residents should be ready to get into the chest almost immediately!
If we have done all of this stuff, sure…do CPR, maybe we’ll circulate some blood through the coronaries…..maybe.
Ultimately, we should consider rapidly terminating resuscitation if these initial maneuvers are unsuccessful, especially in the setting of blunt trauma.
Cheers,
Dillon
Source:
Carenzo, L., Calgaro, G., Rehn, M., Perkins, Z., Qasim, Z. A., Gamberini, L., & Ter Avest, E. (2024). Contemporary management of traumatic cardiac arrest and peri-arrest states: a narrative review. Journal of anesthesia, analgesia and critical care, 4(1), [PubMed]