Utility of BNP in Acute HF?
Hey Team,
I spent 1 hour on shift with you yesterday due to resident conference. But somehow it had me thinking about BNP levels. And I took a look around the internet for an answer to "What does BNP actually do for us in the ED?".
1. What the AHA Says (2022 AHA/ACC/HFSA HF Guideline)
AHA is definitely pro-BNP.
Diagnostic:
Class I recommendation. If a patient presents with acute dyspnea, BNP or NT-proBNP is useful to diagnose or exclude HF.Prognostic:
Also Class I. BNP/NT-proBNP predicts mortality, rehospitalization, and overall risk in HF.Therapeutic guidance:
BNP-guided treatment does not improve outcomes. Not recommended as a target.
AHA summary: BNP is a major diagnostic and prognostic tool.
2. What the Scientific Statement from the ESC HFA, HFSA, and JHFS Says (2023)
This is a multinational consensus from European, American, and Japanese HF societies. Its message strongly reinforces the AHA:
Diagnostic:
BNP/NT-proBNP has very high negative predictive value (94–97 percent) to rule out HF in acute dyspnea.Rule-out cutoffs: BNP <100, NT-proBNP <300.
Prognostic:
BNP is a strong predictor of short- and long-term outcomes.Admission levels predict mortality.
Predischarge BNP predicts 30–180-day rehospitalization.
A 30 percent change from a patient’s baseline is clinically meaningful.
Caveats:
BNP is not specific: renal failure, sepsis, AFib, older age, obesity etc all affect values.
International societies’ summary: BNP is excellent for ruling out HF and good for prognostication.
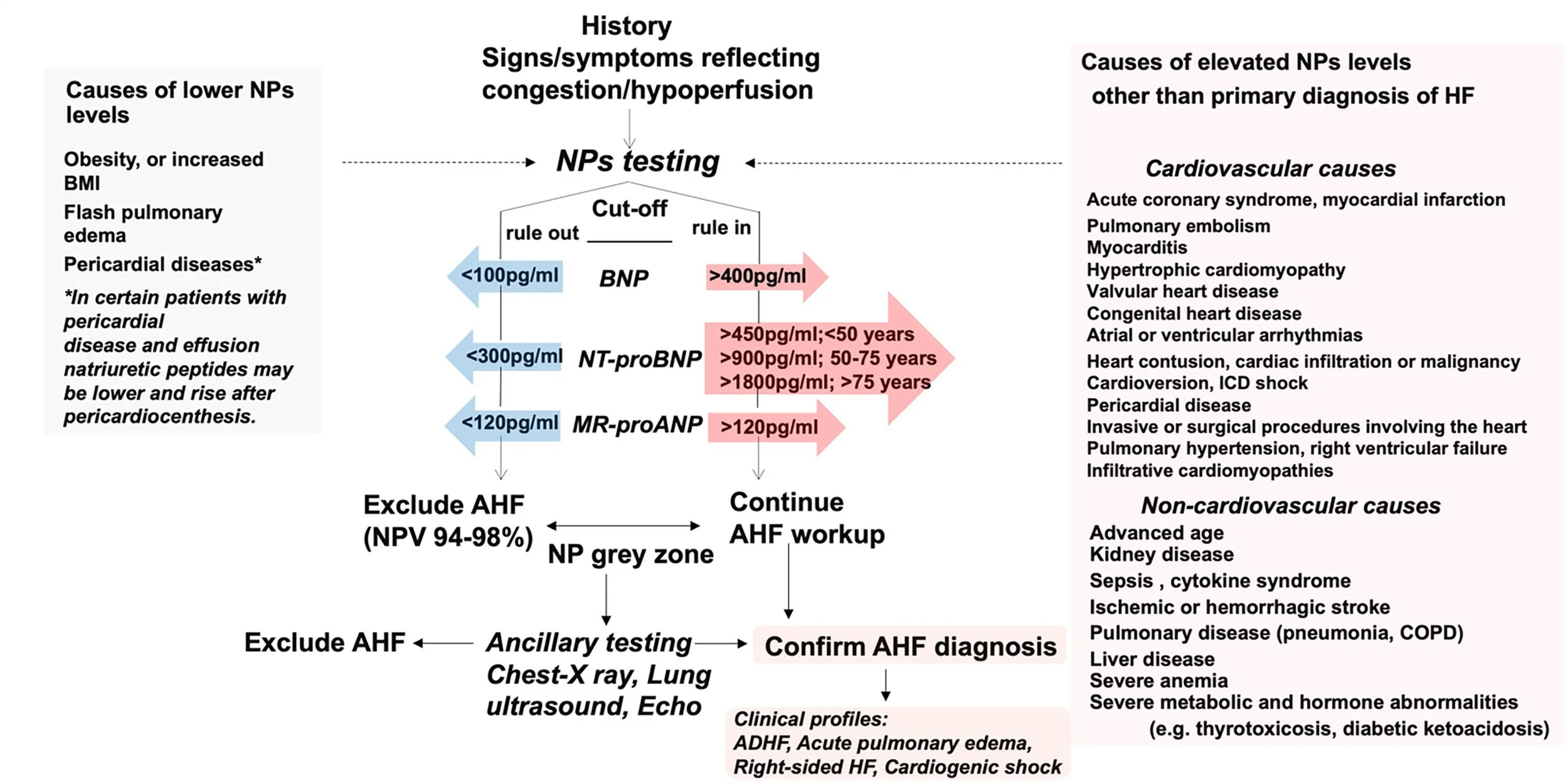
See their Figure 5. Which basically says: In acute dyspnea, a BNP <100 pg/mL or NT-proBNP <300 pg/mL provides an excellent negative predictive value to rule out heart failure, while BNP >400 pg/mL and age-adjusted NT-proBNP cutoffs help rule in the diagnosis, though rule-in thresholds must be interpreted cautiously because many conditions can falsely raise or lower natriuretic peptide levels. About 20 percent of patients land in a gray zone between rule-out and rule-in, and roughly half of these will have acute HF, making clinical features (history of HF, JVP, prior diuretic use) and ancillary testing essential. Interpretation is strongest when compared with the patient’s baseline “dry” BNP/NT-proBNP, since a 25–30 percent change from baseline, indicates a meaningful clinical shift such as decompensation.
3. What ACEP Says (2022 Acute HF Clinical Policy)
ACEP is the most ED-centric (obviously)
There is no specific recommendation for BNP in the policy.
The diagnostic star in the ED is point-of-care lung ultrasound. They basically say that Lung US bests BNP for diagnosis any day of the week
BNP often does not change management when the diagnosis is already obvious.
BNP is considered adjunctive, not foundational, for ED decision-making.
ACEP summary: BNP is optional; use it only when it changes your probability or your plan.
Bottom Line: The ED Take-Home
BNP helps in the ED when:
The diagnosis is uncertain (COPD vs pneumonia vs HF vs COVID).
You’re in the 40–60 percent pre-test probability gray zone (whatever that means to you).
You need a rule-out tool: low BNP makes HF unlikely.
A very high BNP adds weight that HF is contributing or that the patient is higher-risk.
BNP does not help when:
It’s clearly HF based on exam + POCUS.
It’s clearly not HF.
You’re ordering it solely “for the inpatient team” (they can interpret it better, and it rarely changes ED disposition).
Sources
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure. Circulation. 2022;145(18):e895-e1032.
Tsutsui H, et al. Natriuretic peptides in heart failure: a scientific statement from the Heart Failure Association of the European Society of Cardiology, the Heart Failure Society of America, and the Japanese Heart Failure Society. J Card Fail. 2023;29(6):912-934.
American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute heart failure. Ann Emerg Med. 2022;79(5):e1-e39.
Cheers,
Dillon